For many people with asthma, rescue inhalers are a sort of miracle drug. From gasping for air one minute, heart racing, mind foggy, to near immediate relief and calmer breath the next. And yet, roughly ten people die each day from asthma in the U.S. One reason for these largely preventable deaths is that rescue inhalers — this emergency tool, a powerful and effective medicine — can actually stop working, putting people at risk.
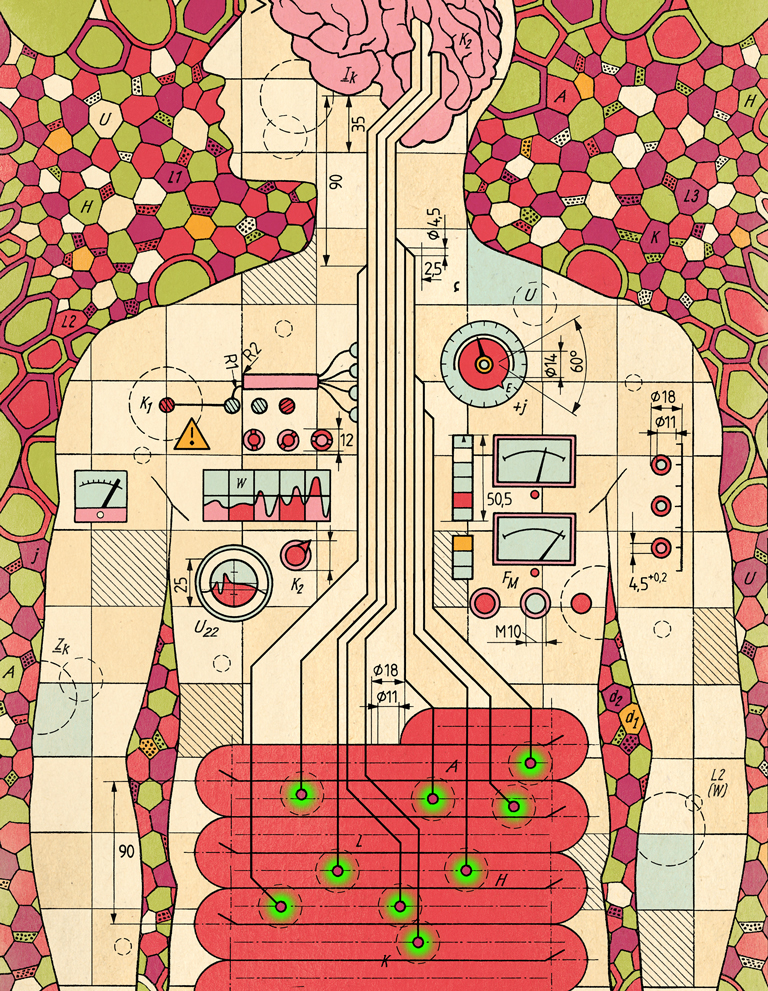
To understand why they stop working researchers zoomed into what was happening on the surface of the cells that line our airways. These cells are covered with little antenna-like molecules sticking through the surface of the cell. These antennae, or receptors, look for signals that tell the cell to change its behavior. In asthma, that antenna is called the beta-adrenergic receptor. When it detects the main ingredient of rescue inhalers, called a beta agonist, it sends two signals: One that’s positive and one that’s a negative side-effect at the crux of rescue-inhaler failure.
The positive signal triggers the cell to relax the smooth muscles of the airway and makes breathing easier. The negative signal turns on a cellular molecule called arrestin, which halts the positive signal, reducing muscle relaxation. With arrestin in place, the beta-agonist can no longer signal muscle relaxation, leaving that lung tissue unresponsive to the next puff from the rescue inhaler, if a need arises too soon.
Two research teams have been working on both sides of the beta-adrenergic receptor’s signals — the positive and the negative — finding ways to tamp down the negative and boost the positive. If these approaches continue to show promise in further tests, they could help reduce death from asthma due to rescue inhaler failure.
For the last decade, biochemist Jeffrey Benovic, PhD, and team have been looking for a way to block the negative arrestin-mediated signal without suppressing the beneficial signals. In a recent study, co-first authors Michael Ippolito, a graduate student, and Francesco De Pascali, PhD, a postdoctoral fellow working with Dr. Benovic and colleague Charles Scott, PhD, found a molecule that did just that in airway smooth muscle cells in mice. After the receptor binds the rescue inhaler’s beta-agonist, Dr. Benovic’s drug would jump in and block arrestin, keeping the antennae ready to receive the next dose of medicine.
In the meantime, another team of researchers were looking at boosting the positive signals that quickly relieve airway constriction. Deepak Deshpande, PhD, and team at the Center for Translational Medicine were looking for a way to make the positive signal and smooth muscle relaxation stronger and active a little bit longer. Most receptors interact with their target briefly, then let it go, essentially halting the signal to relax. But Dr. Deshpande’s group designed a second chemical that would come in and bind another part of the receptor, causing it to change shape slightly and clamp down on the beta-agonist so that the positive signal stays on longer. They were able to show that when their compound was delivered to human cells and in mice along with the beta-agonist, the strength of the drug improved 60-70%, without a comparable increase in arrestin or receptor degradation.
Although it’s unclear whether Dr. Benovic and Dr. Deshpande’s chemicals could be used together, both could potentially improve how rescue inhalers work for people with asthma, when they need them most. The researchers are looking into additional preclinical tests that would make the case even stronger to take these compounds into clinical trials.